Holistic Health

While some choose a term such as Integrative Medicine (IM), which is a form healing – oriented medicine that takes account of the whole person, including all aspects of lifestyle. The term is pejorative at best and most often it is used by someone on the payroll of big medicine or big pharma (yes, the same people who get paid by a company that places a McDonalds or Chick-fil-A in the lobby of their cancer hospital). It emphasizes the therapeutic relationship between practitioner and patient, is informed by evidence, and makes use of all appropriate therapies. By contrast, we are purposely going to use the term “Holistic Health“, which has baggage also, but at least the meaning is less primed with moral hazard. The self imposed definition of Holistic Health is one of scientific rigor agnostically testing the biochemistry of foods and drugs against the bioinformatic markers of the human body. We have no goal, but to get to the correct, mathematically rigorous outcome testing individually in each person with no generalizations.
Facts are that chronic diseases (diabetes, heart disease, alzheimer’s, cancer, cognitive impairment, asthma, obesity, fatty liver disease, osteoporosis, caries (dental cavities), hepatitis, hypertension, stroke, weak or failing kidneys, cystic fibrosis, Arthritis, etc…) have exploded from 30 percent of the population to 60 percent of the population since 1970 in the US. If doctors alone had the solution to the chronic disease epidemic, the numbers would not be as above. If you were the CEO of a company and your profits dropped by 90% as is the equivalent of the increase in the chronic disease rate of the population, you would be fired. Instead, doctors make a bonus the sicker we become. This perverse incentive has been told to me by my doctor acquaintances as “The Pills Pay for the Pool”. Given this scenario and the fact that a doctor is required to have zero nutrition classes to gain a medical degree from Harvard Medical school, we need the rethink the equation.
Medical Schools train physicians how to prescribe drugs that may treat symptoms (25% of a traditional medical school curriculum is pharmacology). Physicians are not trained to address the cause of a chronic disease. In fact, they are paid more if you don’t get better. Would you do any other business deal in your life where the incentives and training was aligned for you to not get well?
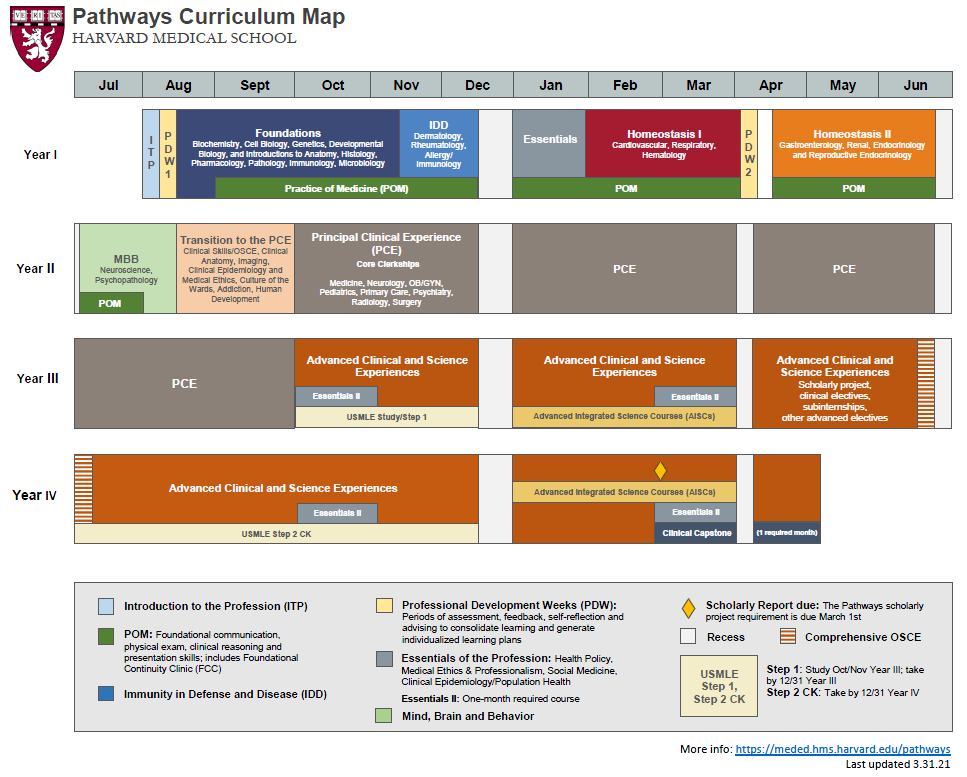
The chart on the left is the full curriculum of a Medical Student at Harvard University (other top schools such as Stanford, Johns Hopkins, etc… are no different).
Let us pause for a moment….Would you fly on an airplane that was built by an engineer who took no classes in mathematics?
Before we address how engineers think about the question above, we will critique the Harvard Medical School Curriculum Map to the left. Notice there is not one single course in nutrition or the science of mathematics. We reason this is almost implausible when a person would be given a task to understand the homeostasis of the human body without training in food intake which is the largest contributor to human health by a factor of 6:1.
A physician acquaintance recently told me in Med School, he was given sick patients and taught to prescribe them drugs to minimize treatment cost. Not once was there any training the the condition was reversible. Not once was there training that the sequence of treatment was only addressing a symptom, not the cause. A doctor is well versed that the big payouts from Medicare and Medicaid don’t come until the patient has renal failure, severe heart disease or latter stage cancer, so what is the incentive to use preventative measures?
You’ve seen it, you’ve heard about it…so what’s the story behind the Iron Ring? In 1900, construction began on the the Quebec Bridge, a bridge which linked Winnipeg to Moncton on the National Trans-Continental Railway. As construction neared completion, it collapsed under the weight of a locomotive loaded with steel. Seventy-five people were killed and a subsequent inquiry showed the accident was due to an error in judgement by the engineers who designed the bridge. Tragedy struck again during the second attempt to build the bridge in 1916. The centre span collapsed while being hoisted into place, killing 10 more people. The bridge was finally completed in 1917. Contrary to popular belief the first rings were not made from iron from the collapsed bridge. But the collapse of the bridge led to the tradition of the Iron Ring to symbolize the humility and fallibility of engineers.
Upon last review, there was something named the Hippocratic Oath, but the oath has turned meaningless if the doctor must pit the private education of their children (from excessive procedures) against the well being off their patients (by encouraging zero revenue preventative care).
The engineer’s iron ring

While it may seem we are hammering physicians and the training they receive from medical schools, the numbers are simply numbers and facts. Not only calling out physicians, the top fortune 1000 CFOs were asked to guess the return of the S&P 500 12 months later. None of them got it right. To ask these same CFOs a 80% confidence interval, less than 30% were correct. If legal outcomes were aligned as such, we would make the same arguments. If medical outcomes were backed by data in patient recovery, we will say so. Such favorable health outcomes do exist, but when a hospital employs 100 oncologists to 1 integrative medicine or nutrition professional and they have a McDonalds or Chick-fil-A in the lobby of the cancer hospital, one would be a fool not to question incentives. One anonymous CFO of a large hospital system recently told me when asked if they would like a technology based health solution for employees and patients: “Our average patient and employee has 2-3 cokes a day and fast food for lunch, they are overweight and many have diabetes, why would we want change? We make more revenue if things stay the same.”
Some physicians are willing to tell the truth, albeit rare and few and far between. Dr. Robert H. Lustig MD (trained at Cornell Medical School) recently wrote a semi-lucid book as a recovering physician after 30 years in the industrial medical complex: “Academics and clinicians nationwide stand by both modern medicine and our healthcare system. They feel that investing in areas such as “personalized medicine” technologies that “cure” people diagnosed with cancer, cardiovascular diseases, or neurological diseases will ultimately yield better long-term results than focusing on public health measures. This conclusion is wrong, both at the individual level and societal levels, and show at best the misconception of what the real problems are, and at worst a perverse desire of the various stakeholders to maintain the status quo at the expense of both lives and dollars. We spend 97.5 percent of our healthcare budge on individual treatment, and only 2.5 percent on prevention. Not a very good bang for the buck. Here are six clear reasons why we need to rethink modern medicine” Lustig, Robert. “Metabolical” HarperCollins, 2021, p 19-20:
- Which is better? To be cured of cancer or not to get cancer at all? Only 33 percent of the people treated for cancer are “cured” as defined by 5+ years of survival post diagnosis.
- Over the past twenty years, the National Cancer institute has spent $60 Billion on research and treatment, yet only 7% remain cancer free for 20 years. Nearly all “cancer cures” are priced at $100,000 to $500,000 with the aforementioned abysmal results.
- Take Alzheimer’s research at $2.5 Billion a year with over 100 drugs tested and discarded. In fact Pfizer wrote off billions recently stating they were wrong that Alzheimer’s was “genetic”, but rather it is “metabolic” (what we eat).
- Only 13 percent of those 54 years old report they are in “good health” as opposed to 32 percent in 1988.
- Our healthcare system is collapsing as the cost are unsustainable for both business and government to support. in 1980 30 percent of adults (54 million people) reported one chronic condition. Today that number is 145 million or 60 percent. The percentage of those effected by two or more chronic diseases has grown from 16 percent to 42 percent.
- On average patients with 5 or more chronic diseases spend 14 times more on health services than those with no chronic condition.
World Healthcare Figures
World Life Expectancy
While the US is number 1 in healthcare cost per capita by 50%, the US ranks 50th in the world for life expectancy. The US ranks 44th in infant mortality rates. How is it possible to spend so much, but end up with mediocre results?
While evaluating science based outcomes, we must step back to use true analysis rather than our “expert judgement”. In the wake of the 9/11 terroist attacks, the death toll stood at 2,996 including the 19 hijackers, but research suggests that there is a further, indirect toll as a result of behavioral changes induced by fear. In the months after the 2001 terror attacks, passenger miles on the main US airlines fell by between 12% and 20%, while road use jumped. The change is widely believed to have been caused by concerned passengers opting to drive rather than fly. Travelling long distances by car is more dangerous than travelling the same distance by plane. Measuring the exact effect is complex because there is no way of knowing for sure what the trends in road travel would have been had 9/11 not happened. However, Professor Gerd Gigerenzer, a German academic specialising in risk, has estimated that an extra 1,595 Americans died in car accidents in the year after the attacks – indirect victims of the tragedy.
Annenberg University Professor at the University of Pennsylvania Philip Tetlock has written numerous papers showing the predictive abilities of physicians for complex cases may be below 40% in reviewing diagnosis compared to autopsies.
“A total of 118 physicians with broad geographical representation within the United States correctly diagnosed 55.3% of easier and 5.8% of more difficult cases (P < .001) (making an overall average of a 31% success rate). Despite a large difference in diagnostic accuracy between easier and more difficult cases, the difference in confidence was relatively small (7.2 vs 6.4 out of 10, for easier and more difficult cases, respectively) (P < .001) and likely clinically insignificant. Overall, diagnostic calibration was worse for more difficult cases (P < .001) and characterized by overconfidence in
accuracy” (p. 1952) (Ashley, N. D., Meyer AND, Payne VL, Meeks DW, et al. Physicians’ Diagnostic Accuracy, Confidence, and Resource Requests. JAMA Internal Medicine. 2013; 173 (21): 1952 – 1958 ) Another major, and more disturbing finding of the Ashley’s et al. study, was how little the physicians’ level of confidence changed from the easy to the hard cases (7.2 out of 10 for the easy ones and 6.4 out of 10 for the hard ones). This means that with an accuracy rate of only 5.8%, the physicians were still 64% confident that they had come up with the right diagnosis! In terms of decision making, a low diagnostic accuracy of 5.8% could have been tolerated if the physician was, say, only 10% confident of being right. In that case she could have been ordering more tests, reevaluating the symptoms, or asking for a second opinion from another doctor in order to improve the chance of a correct diagnosis. However a 64% confidence probably excludes such actions, convincing the doctor to proceed with a treatment, based on the wrong diagnosis, the consequences of which could be harmful for the patient.
Fink, Lipatov and Konitzer attribute the reasons for such overconfidence in the doctors’ judgment to the well-known “expert” problem saying that “most practitioners believe that they have valuable experience and precious intuition. However, simple logic shows that all of their experience is still only a small (often biased!) sample” (Fink W, Lipatov V, Konitzer M. Diagnoses by general practitioners: Accuracy and reliability. International Journal of Forecasting. Science Direct. 2009; 25: 784 – 793) . Thus, it seems that the common problem of overconfidence encountered in the field of forecasting is also present in medical diagnoses with detrimental negative outcomes and an urgent need for concrete steps to correct it as people’s wellbeing and lives are seriously affected. In his PLoS Medicine article Loannidis states: “There is increasing concern that in modern research, false findings may be the majority or even the vast majority of published research claims” (p. [696) (Ioannidis JP. Why most published research findings are false. PLoS Medicine. 2005; 2:e124.). In his article in JAMA, he concludes “Contradiction and initially stronger effects are not unusual in highly cited research of clinical intervention and their outcomes” ( Ioannidis, JP and Lau, J. Evidence on Interventions to reduce Medical Errors; An Overview and Recommendations for Future Research, Journal of General Internal Medicine. 2001; 16 (5): 325 – 334. doi: 10.1046/j.1525-1497.2001.00714.x ) (Ioannidis JP. Contradicted and initially stronger effects in highly cited clinical research. JAMA Internal Medicine, 2005; 294: 218 – 228.)(p. 218). In a 2010 article in the Atlantic featuring Ioannidis, Freedman quotes him saying “that as much as 90 percent of the published medical information that doctors rely on is flawed and that he worries that the field of medical research is so pervasively flawed, and so riddled with conflicts of interest, that it might be chronically resistant to change—or even to publicly admitting that there’s a problem”.
What does the chief medical officer of the American Cancer Society Say?
Dr. Brawley as the chief medical officer of the American Cancer Society teaches about the racism and unequal opportunities for those on Medicaid vs. private insurance. While his analysis is accurate to teach important disparities, it also shows how doctors think of themselves as unable to “cure” because of patients who are afraid, ignorant or limited by insurance options. This analysis also illustrates how physicians are trained to “treat symptoms” rather than stepping back to be part of the solution which means less medicine and more prevention. The cost of prevention has never been cheaper with improvements with remote diagnostics, but doctors and the system need reform.
Surely Brawley brings a wealth of well grounded experience from the Grady Public Hospital in Atlanta. He mentions issues with “food deserts and poverty” effecting the age of menstruation of inner city youth which then in turn effects breast cancer rates. After spending many years ourselves volunteering in the homeless shelters of America, spending summers of missionary work in India, Pakistan and West Africa, be assured a “food desert” in Atlanta is not the issue. Later, we will demonstrate with the tap of the smart phone in India, Africa or inner city Atlanta, the spinach can be flowing. It is as simple as a little more “spinach” and less “McDonalds” at the hospital. By the way, WTF is Ronald McDonald House doing in the Cancer Ward at MD Anderson in Houston ? Or Chick-fil-A doing at Grady Memorial Hospital in Atlanta?
Again, let us step back and listen to even what clinician leaders are taking to the pen to write such as Otis Webb Brawley who led the American Cancer Society in his book “How we do Harm: A doctor breaks ranks about being sick in America.”
How We Do Harm exposes the underbelly of healthcare today—the overtreatment of the rich, the under treatment of the poor, the financial conflicts of interest that determine the care that physicians’ provide, insurance companies that don’t demand the best (or even the least expensive) care, and pharmaceutical companies concerned with selling drugs, regardless of whether they improve health or do harm.
Dr. Otis Brawley is the chief medical and scientific officer of The American Cancer Society, an oncologist with a dazzling clinical, research, and policy career. How We Do Harm pulls back the curtain on how medicine is really practiced in America. Brawley tells of doctors who select treatment based on payment they will receive, rather than on demonstrated scientific results; hospitals and pharmaceutical companies that seek out patients to treat even if they are not actually ill (but as long as their insurance will pay); a public primed to swallow the latest pill, no matter the cost; and rising healthcare costs for unnecessary—and often unproven—treatments that we all pay for. Brawley calls for rational healthcare, healthcare drawn from results-based, scientifically justifiable treatments, and not just the peddling of hot new drugs.
Brawley’s personal history – from a childhood in the gang-ridden streets of black Detroit, to the green hallways of Grady Memorial Hospital, the largest public hospital in the U.S., to the boardrooms of The American Cancer Society—results in a passionate view of medicine and the politics of illness in America – and a deep understanding of healthcare today. How We Do Harm is his well-reasoned manifesto for change.
If traditional medicine is broken, what is the solution?
As we can observe from the data above, many doctors are simply not qualified to to make the decisions they make (be it for immoral hazard or lack of training). Certainly some are qualified, but to see a doctor recommend a course of preventative treatment while foregoing prescription revenue and follow up visit revenue is nearly unheard of. Paying a doctor if your treatment is successful would help correct the immoral hazard, but have you ever had a doctor offer you such a proposition? More likely they make sure you have some money left in your property assets before they help move you to palliative care to make sure your inheritance to your children has been wiped out. If this angers a physician, take the other side and only pay yourself if your patient improves from a standard you both agree upon. Such a proposition would be viewed as welcome from your patients.
Assuming physicians won’t be part of the solution (which we welcome them being part of the solution), a viable solution is insurance with biometric testing to provide incentives for holistic health performance. While people don’t follow diets, they do perform for money.
Our solutions with CirclesX Health provide such incentivized solutions and the technology to assist in the search and delivery of food to help the body heal. We help align dietary, exercise, sleep, walking patterns with health outcomes that will target “Foodie Body Zone” Membership rewards.
While we are not adverse to science based medicine backed by independent data proving a superior outcome to preventative care, it is the responsibility of the physician to present this to the patient with indpendent data, not because the pharma rep brought lunch or reviewed a study by the seller which has not been vetted by independent peers.
Nutrition Unpacked
Foodie Body search engine on the CirclesX platform helps users upload their latest labs in PDF or electronic format in their user profile. Once your labs are uploaded and associated with your profile, the search engine will recommend recipes and food for delivery which are optimized for your biochemistry.

INTERESTING FACT:
The influence of diet in pregnant women on the immune tolerance process is intricate. Food-specific immunoglobulin G (IgG) was associated with exposure to particular food antigens. The IgG antibodies can cross the placental barrier and enter into the colostrum, and maternal IgG is amply present in breast milk. This justifies studying the immunological connection between food-specific IgG antibodies and the mother–fetus relationship.
Eat foods such as nuts, dark green leafy greens, sweet potatoes and avocado to get more vitamin E in your meals. Vitamin E is known to boost immunoglobulins. As diet and our trips to the grocery store tend to be based on “System 1” thinking where we see words that may seem healthy, we really need to approach our eating using our “System 2” thinking. While looking at a nutrition label may seem like multiplying 24 x 57 in your head (we can’t do this using system 1 thinking), we have designed Foodie Body Search so that you upload your blood labs and then just type a food and the system does all the “System 2” math for you. The benefit is you can get an instant “System 1” decision or information quickly, while outsourcing all the “System 2” math to the Foodie Body Search engine.
Disease Prevention
Customized Solutions for your body and chemistry
Just as epigenetics can cause issues such as metabolic syndrome, cancer, heart disease, mental disorders, auto-immune disease and diabetes, food can also ameliorate these conditions. To learn more on if the first steps of a plant based whole foods plan are right for you create a free account and review the 30 day Foodie Body plan. There is no charge to participate and the search engine will customize your food results to help improve your independently verified labs. Consult your physician before commencing on a dietary change to ensure it is right for you.
Biochemistry

Holistic Health
CirclesX LLC
a SimpsX Technologies LLC company
12335 Kingsride Lane #418
Houston, Texas 77024
Technical Support (832) 916-2001
Geolocation Exchange Markets and Search

